DHA & IMMUNITY
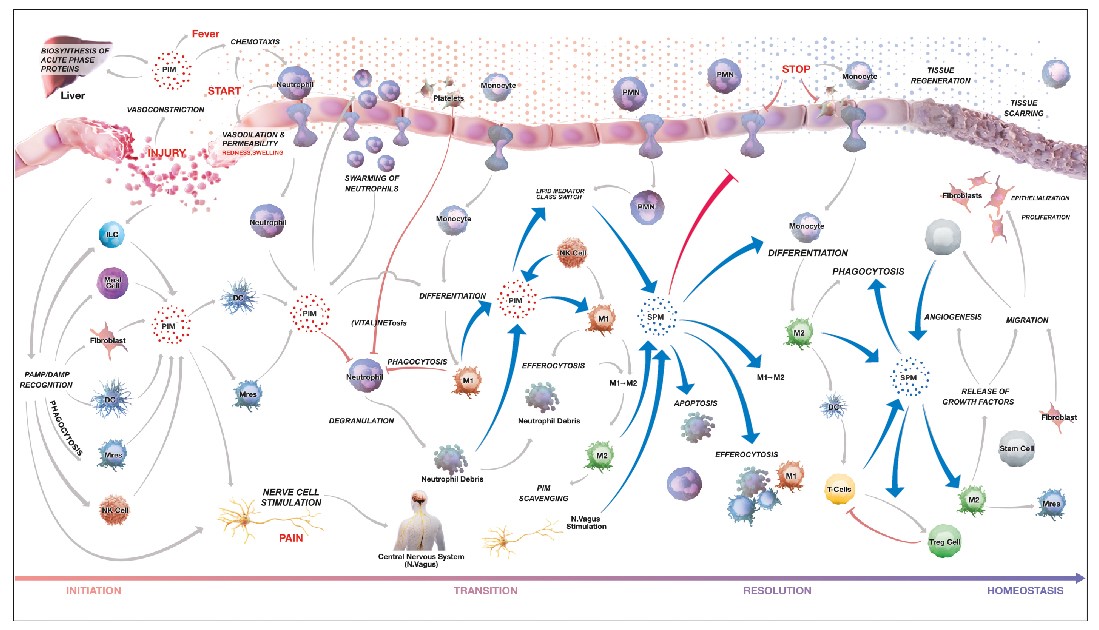
The immune system is a complex series of barriers, mechanisms and responses that help our bodies deal with infection, injury and malfunctioning cells such as tumours. It involves a wide variety of cells distributed throughout our bodies that interact to identify and respond to threats either systemically or locally. Reacting to stimuli is an important function of the system, but equally not reacting to non-harmful stimuli and resolving and terminating responses when they are no longer appropriate is also critical.
Innate responses include physical barriers to entry of pathogens, mechanisms to recognise common biochemical markers associated with infection, and mechanisms such as inflammation, and phagocytosis which can be used to deal quickly with a large variety of infections.
Adaptive responses are far more specific and involve antibodies and specific cell types (B cells and T cells) that can recognise antigens associated with particular diseases. While effective, these responses are slower to act than the innate system.
While the immune system has evolved to prevent acute disease from infection, inappropriate activation be the cause of many chronic diseases, including autoimmune diseases such as lupus or rheumatoid arthritis where the body reacts to itself, or inappropriate intolerance to, for example, our natural gut microorganisms causing bowel diseases.
With such a complex system it is unsurprising that proper nutrition, especially of micronutrients such as vitamins, minerals and the polyunsaturated fatty acids docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA), can have a major impact on the ability of our immune response to react appropriately and effectively2,3. This has been recognised since the days of scurvy, although the mechanisms (vitamin C deficiency) took a little longer to work out.
Even today, our understanding of the mechanisms of the immune system are growing and with the arrival of the SARS-CoV-2 virus and COVID-19 there is an obvious interest in optimising our immune function.
Prevention is better than cure and actions such as hand-washing, mask wearing and vaccination are in the forefront of our response to COVID-19, and have also led to a reduction in other infectious diseases over the same time. Nonetheless, ensuring proper immune function through proper nutrition could reduce the load on the medical system through reduced hospitalisation from all infection and have a significant positive benefit for the wellbeing of the population as a whole4.
Figure 1: Pathways of inflammation and its resolution. From the Atlas of Inflammation Resolution(1).
The role of omega-3s in the immune system
DHA and EPA appear to have at least three major roles in the immune system, most of which appear to be linked with ensuring that the immune system responds appropriately to triggers and returns to a quiet state once infections have been resolved. This is not a suppression of the immune system, but an integral part of its correct function5.
With our minds currently focussed on viral infection, resolving the immune response after infections have been cleared may not seem as important as initiating the response to infection in the first place, but unresolved inflammation is at the root of a wide variety of chronic diseases with long term impacts on health and quality of life. Inappropriately regulated responses can also lead to danger during infection with an overactive immune system responsible for the ‘cytokine storm’ at the root of acute respiratory distress seen with COVID-196. Omega-3s thus clearly have an important role in keeping our immune systems fighting-fit.
Incorporation into membranes
As we saw in an earlier newsletter on brain and eye health, DHA and EPA can play an important structural role in membranes. These fatty acids are rapidly incorporated into the membranes of cells of the immune system7, with increased levels seen after even a day of supplementation and peaking after only a few weeks.
If these levels can be maintained by appropriate levels of intake, they already serve one important purpose by supplanting the fatty acid arachidonic acid (AA) in cell membranes. AA is one of the omega-6 fatty acids and is the starting molecule for the synthesis of a number of pro-inflammatory compounds. By replacing AA with omega-3s, the level of these compounds is decreased8.
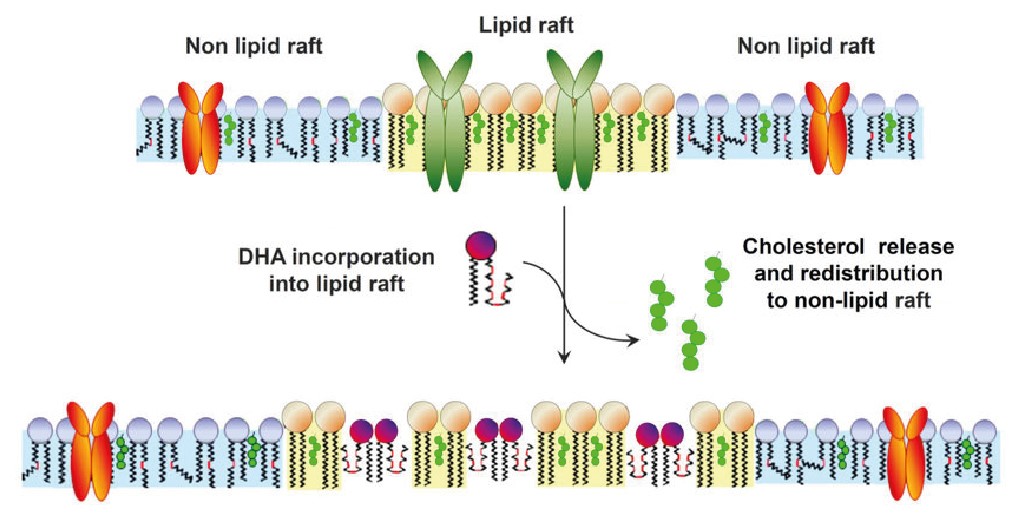
The presence of the omega-3 fatty acids, especially DHA, can also alter the structure of the membranes of these immune cells. Areas of the cell membrane involved in signalling often involve ‘rafts’ of relatively immobile groups of proteins held in place with cholesterol that interact with each other to trigger inflammatory signals. Due to DHA disrupting cholesterol structures in the membrane, DHA disperses these rafts and reduces the level of signalling9 thus modulating the responses to infection and injury.
Figure 2: DHA’s impact on lipid raft structures(10).
Omega-3 impacts gene expression of genes associated with immune response
Whether through their impact on membrane structures or other routes, EPA and DHA have a clear impact on the expression of genes. A study carried out in healthy volunteers aged 65 years and older showed that over a thousand genes had their levels of expression changed in cells of the immune system after 26 weeks of supplementation with omega-3s, and the level of the effect depended on the dose taken11. Roughly half of these were down-regulated (expression was decreased) including many associated with inflammatory pathways. These included genes responsible for the transformation of ARA to pro-inflammatory compounds indicating that the positive effects of EPA and DHA are not just the result of displacement of AA from cell membranes.
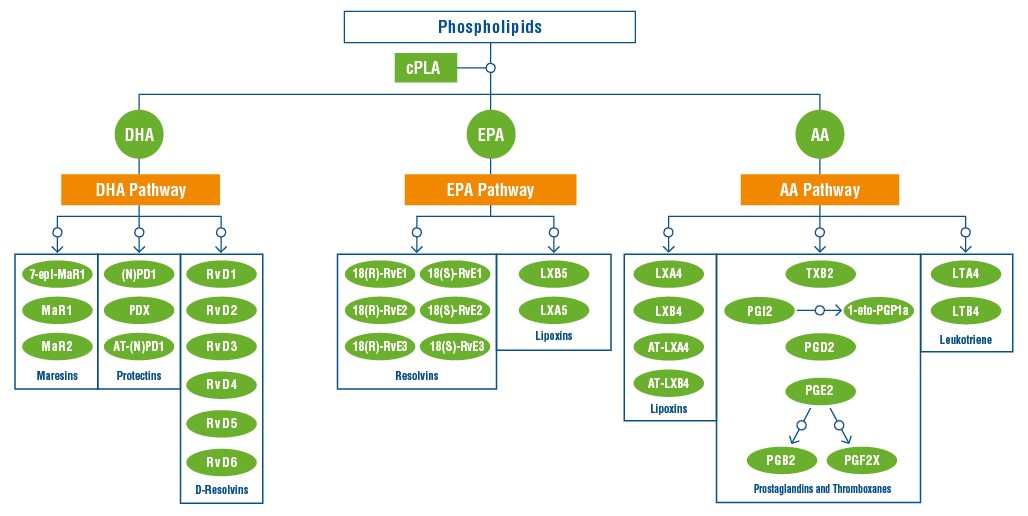
DHA as a precursor for active metabolites
Polyunsaturated fatty acids are not just structural components of cell membranes, but are precursors for a number of different bioactive molecules12. As previously mentioned, the omega-6 arachidonic acid is transformed into molecules with pro-inflammatory actions such as the Prostaglandins and Thromboxanes, or the Leukotrienes involved in signalling within the inflammation response. Some of its metabolites, however, also have an inflammation resolving effect, notably the Lipoxins. EPA is transformed into inflammation-resolving Lipoxins and Resolvins, while DHA is transformed into three families of bioactives:
-
-
-
- Maresins, involved in resolving inflammatory and allergic reactions, in wound healing, and in abating neuropathic pain
- Protectins, which have a potent anti-apoptotic and anti-inflammatory activity; and
- D-Resolvins, which help promote the restoration of normal cellular function following inflammation.
-
-
Figure 3: Generation of inflammation mediators from polyunsaturated acids. From the Atlas of Inflammation Resolution.(1)
Ensuring the best nutrition for your immune system
We are gaining more and more insight into how a healthy diet can impact both your immediate health and long-term wellbeing and our immune systems are no different. Ensuring complete nutrition while at the same time living sustainably and respecting the planet can be hard, especially for those choosing to reduce or eliminate meat intake or avoid fish. Omega-3 supplementation is an effective method of ensuring that we consume enough of these essential fatty acids. For a truly sustainable option, compatible with both vegan and vegetarian diets, algal DHA is a great solution that can boost not only the amount of DHA in the blood, but also EPA13.
Fermentalg’s DHA ORIGINS™ range consists of oils containing very high levels of DHA and which can be taken to provide up to 1g of DHA per day in Europe, permitting your clients to maximise the health benefits in a small form-factor.
Bibliography :
- Serhan, C. N. et al. The Atlas of Inflammation Resolution (AIR). Mol. Aspects Med. 74, 100894 (2020).
- Gombart, A. F., Pierre, A. & Maggini, S. A Review of Micronutrients and the Immune System–Working in Harmony to Reduce the Risk of Infection. Nutrients 12, 236 (2020).
- Calder, P. C., Carr, A. C., Gombart, A. F. & Eggersdorfer, M. Optimal Nutritional Status for a Well-Functioning Immune System Is an Important Factor to Protect against Viral Infections. Nutrients 12, 1181 (2020).
- Messina, G. et al. Functional Role of Dietary Intervention to Improve the Outcome of COVID-19: A Hypothesis of Work. Int. J. Mol. Sci. 21, 3104 (2020).
- Jaudszus, A. et al. Evaluation of suppressive and pro-resolving effects of EPA and DHA in human primary monocytes and T-helper cells [S]. J. Lipid Res. 54, 923–935 (2013).
- Szabó, Z. et al. The Potential Beneficial Effect of EPA and DHA Supplementation Managing Cytokine Storm in Coronavirus Disease. Front. Physiol. 11, 752 (2020).
- Kew, S. et al. Effects of oils rich in eicosapentaenoic and docosahexaenoic acids on immune cell composition and function in healthy humans. Am. J. Clin. Nutr. 79, 674–681 (2004).
- Calder, P. C. n-3 Fatty acids, inflammation and immunity: new mechanisms to explain old actions. Proc. Nutr. Soc. 72, 326–336 (2013).
- Shaikh, S., Rockett, B., Salameh, M. & Carraway, J. K. Docosahexaenoic Acid Modifies the Clustering and Size of Lipid Rafts and the Lateral Organization and Surface Expression of MHC Class I of EL4 Cells. J. Nutr. 139, 1632–9 (2009).
- Corsetto, P., Colombo, I., Kopecka, J., Rizzo, A. & Riganti, C. ω-3 Long Chain Polyunsaturated Fatty Acids as Sensitizing Agents and Multidrug Resistance Revertants in Cancer Therapy. Int. J. Mol. Sci. 18, 2770 (2017).
- Bouwens, M. et al. Fish-oil supplementation induces antiinflammatory gene expression profiles in human blood mononuclear cells. Am. J. Clin. Nutr. 90, 415–424 (2009).
- Duvall, M. G. & Levy, B. D. DHA- and EPA-derived resolvins, protectins, and maresins in airway inflammation. Eur. J. Pharmacol. 785, 144–155 (2016).
- Schuchardt, J. P. et al. Effects of docosahexaenoic acid supplementation on PUFA levels in red blood cells and plasma. Prostaglandins Leukot. Essent. Fatty Acids 115, 12–23 (2016).